Heart failure, as you may know, is a condition where the heart fails to pump blood efficiently leading to shortness of breath, fatigue, weakness, swelling in the limbs, rapid or irregular heartbeat, persistent cough, loss of appetite and nausea. You may read our earlier article to better understand the causes and types of heart failure:
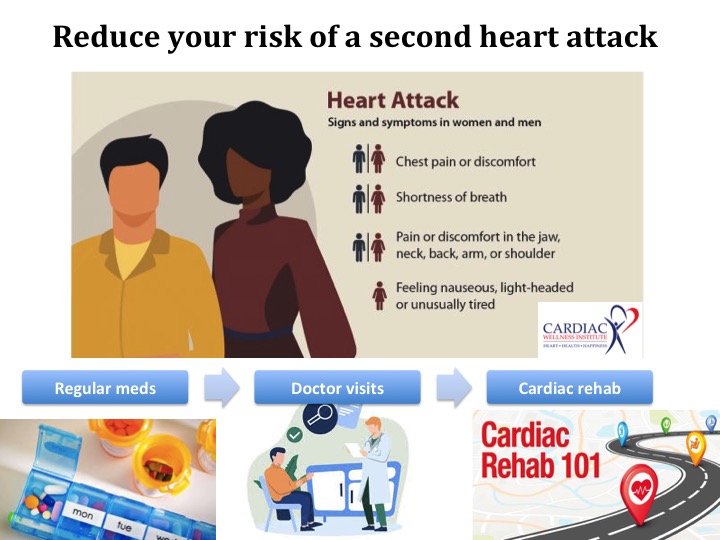
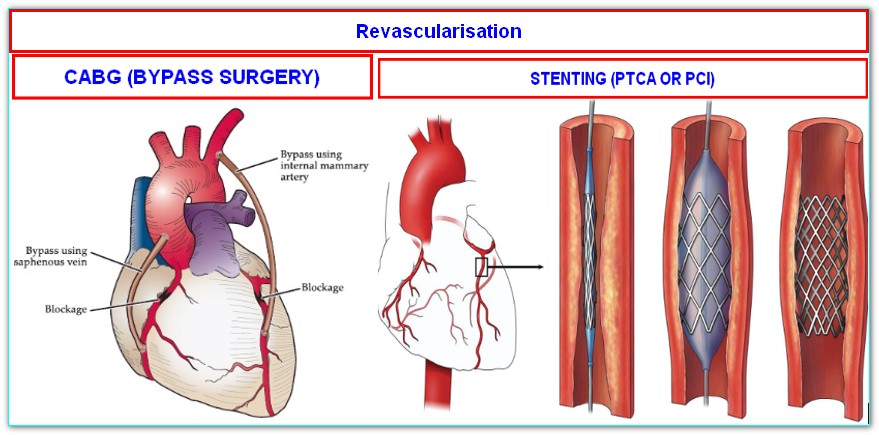
We now know that cardiac rehabilitation or cardiac rehab is the best therapy for heart failure, especially when combined with the right medications and surgical or interventional procedures as needed.
What is Cardiac Rehabilitation?
Cardiac rehabilitation is a program designed to help people with heart problems recover, improve their overall health and reduce the risk of future heart problems. It is a team effort involving healthcare professionals such as cardiologists/ physicians, nurses, physiotherapists, dietitians and psychologists.

What are the phases of Cardiac Rehabilitation?
Phase 1: Inpatient Phase (in the hospital)
Patients with heart ailments such as heart failure might be referred to cardiac rehabilitation right from their hospital stay. The rehab team will assess and evaluate your physical as well as psychosocial abilities and initiate education, early mobilisation, medications and lifestyle modifications.
Phase 2: Outpatient Phase (post discharge)
Once the patient is discharged from the hospital, the rehabilitation will continue at an outpatient care facility. It involves supervised exercise training, education on risk factor management, nutritional guidance, psychological counselling and lifestyle changes.
Phase 3: Training Phase
It focuses on long term cardiovascular health maintenance and involves transition from supervised to a less supervised exercise training.
Phase 4: Maintenance Phase
This phase continues throughout your entire life once you complete the previous 3 phases. Patients are encouraged to make regular exercise a part of their daily routine and adopt healthy lifestyle choices.
How is Cardiac Rehabilitation beneficial in heart failure patients?
- Makes the cardiovascular system stronger
- Improves exercise capacity
- Enhances quality of life
- Reduces hospital readmissions
- Improves long term adherence to healthy behaviours
- Helps control the risk factors which lead to heart failure (e.g., diabetes, hypertension, etc.)
- Elevates mood and positive attitude towards life
What are the safety measures to be followed during exercise?
- Consult with your physician before starting or modifying an exercise routine
- Start gradually and progress slowly
- Prior to exercise, perform a warm-up routine and end the session with a cool-down period
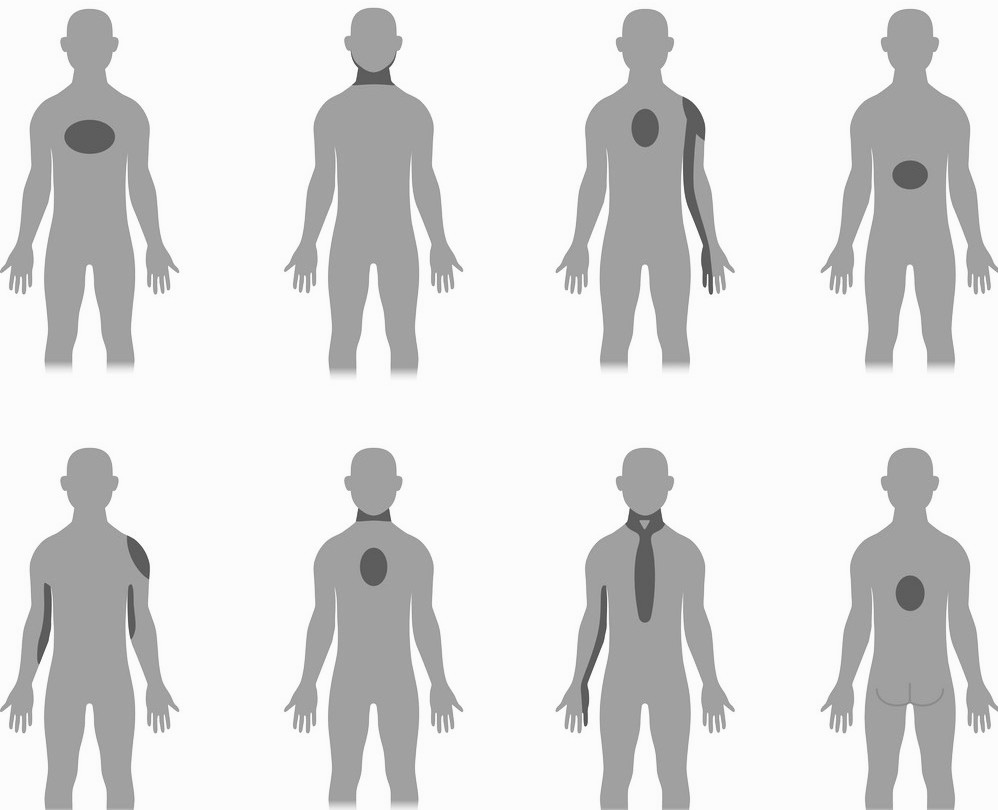
- Keep track of your heart rate and symptoms such as chest pain, palpitations, shortness of breath, dizziness, leg cramps and excessive fatigue
- Stay hydrated, consuming fluids as advised by your physician
- Take prescribed medicines as directed
- Exercise in a safe and controlled environment
Hence, enrolling in a cardiac rehab program is a positive step towards taking control of your heart health and enjoying a better quality of life. Remember that you are not alone in this journey, and there is a dedicated team ready to support you in every possible way.