- What is cardiac rehab?
Cardiac rehabilitation or cardiac rehab is nothing but a medically supervised program to help individuals with heart diseases get back to normal health and routine activities as early and safely as possible. A cardiac rehab program is an exercise cum education program individualised to the medical, psychological and social needs of the participants.
- Why is it gaining importance?
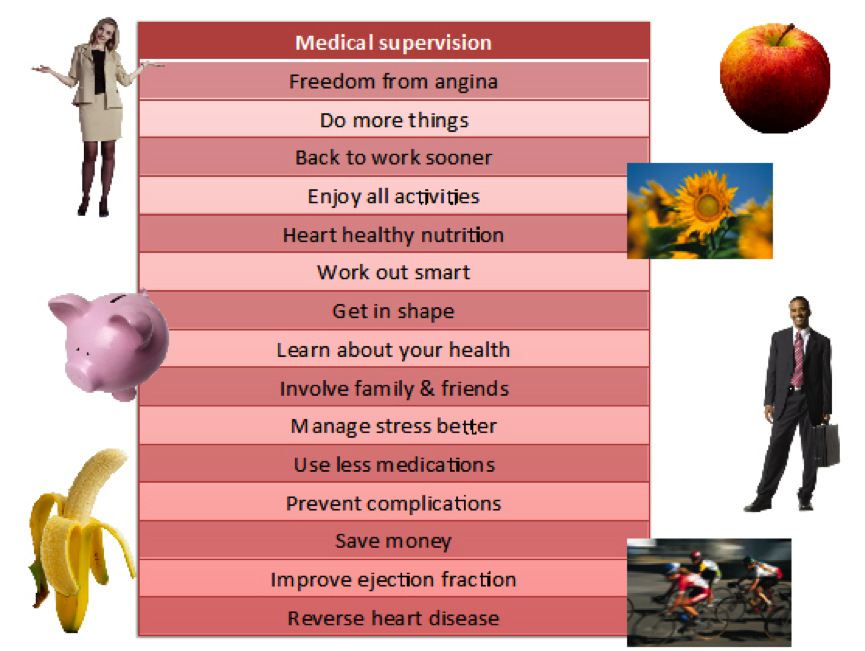
Several research studies from the recent past have demonstrated that individuals who undergo cardiac rehab have better immediate and long-term outcomes as compared to those who do not receive cardiac rehab. The benefits of cardiac rehab are improvement in risk factor control, positive changes in health-related behaviour, increased physical ability to do things, better psychological wellbeing and disease coping skills, and a reduction in symptoms, repeat hospitalisations and complications. The American Heart Association, the European Society of Cardiology and the British Cardiovascular Society recommend that all eligible individuals should be referred for cardiac rehabilitation.
3. Who is eligible for cardiac rehab?
Individuals with one or more of the following conditions are eligible for cardiac rehab: coronary heart disease (blocks in the blood vessels supplying the heart), angina (chest pain on exertion), angioplasty (stenting), bypass surgery (coronary artery bypass graft or CABG), heart failure, heart valve surgery, heart transplantation and device implantation.
- How is cardiac rehab provided?
Cardiac rehab centres may be housed within a hospital or they may be located in the community as outpatient units. The program is typically provided by a multidisciplinary team of healthcare professionals, which includes a physician, a physiotherapist, a nutritionist and a counselling psychologist.
There are typically 4 phases and 4 components in a cardiac rehab program:
Phase 1 – guidance and counselling during hospitalisation (the rehab team will meet the affected individual and his/her family and provide clarification about the health condition)
Phase 2 – monitoring and support during the recovery period (which might be just a few days for a stent procedure and about 6 weeks for bypass surgery)
Phase 3 – supervised exercise cum education sessions (participants will attend two or three sessions a week for 6-12 weeks)
Phase 4 – maintenance and follow-up (upon completion of the program, participants will continue to adhere to the lifestyle changes at home and visit the rehab centre periodically)
- When should one enrol in a cardiac rehab program?
Enrolment in a cardiac rehab program is best done immediately after a heart disease is diagnosed (such as myocardial infarction or heart attack) or after an intervention or surgery (such as stent placement or bypass surgery). Having said this, not everybody would have easy access to a cardiac rehab facility. Nevertheless, participating in a cardiac rehab program any time after a cardiac event or procedure will lead to better outcomes than not doing so.
- Are there any side effects or hazards of cardiac rehab?
Cardiac rehab is generally safe, especially when safety guidelines are adhered to and participants are grouped according to their risk. There is a very small risk of adverse effects such as rhythm problems or injuries but the benefits far outweigh the risks. The rehab team will explain about the warning signals to look for when exercising and ensure that rehab participants exercise safely during the sessions as well as at home.
- How are the benefits of cardiac rehab assessed?
Some of the assessment tools used pre-program and at end-of-program are questionnaires to assess health-related behaviour, psychosocial wellbeing and nature and frequency of symptoms, anthropometry (weight, body mass index, waist hip ratio etc.), blood pressure, blood biochemistry (blood sugar, cholesterol levels), functional capacity (ability to exercise) and ejection fraction (an echocardiographic assessment of heart function).
- What happens after a cardiac rehab program?
Upon completion of a cardiac rehab program, individuals will be put on a maintenance program whereby periodic visits to the rehab centre will pave the way for better long-term adherence and adequate clinical monitoring.
- Is cardiac rehab an alternative to medications, stenting or bypass surgery?
Cardiac rehab is not a replacement for medications, stenting or surgery. It is a more holistic approach to treatment addressing the root cause of disease rather than just the symptoms and signs.
- How to get further information about cardiac rehab?
The following links give useful and reliable information:
http://www.nhlbi.nih.gov/health/health-topics/topics/rehab
https://www.bhf.org.uk/heart-matters-magazine/wellbeing/cardiac-rehab
You could visit our website www.cardiacwellnessinstitute.com or contact us for any clarifications or additional information about cardiac rehabilitation in India.
Author:
Dr. Priya Chockalingam, MBBS, MRCPCH, PhD Cardiology cardiacwellnessinstitute@gmail.com, Phone: +91 9940408828, +9144 43192828
