For someone who has suffered a heart attack, has gone through several tests and life-saving procedures and has a long list of medicines to consume, a diagnosis of heart failure can be depressing. It not only means more medicines and more investigations but also lesser ability to do the things they enjoy and a reduced quality of life. However, the outlook for individuals with heart failure is not so gloomy after all. In fact, if you read this post till the end, you will be convinced that there is so much one can do to manage heart failure better!
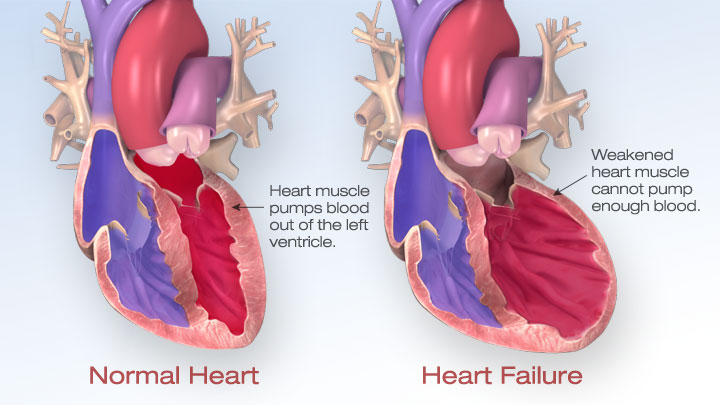
The term ‘heart failure refers’ to the inability of the heart to perform its work well. In other words, the heart is not pumping blood effectively leading to all the body parts getting lesser oxygen than they need. The causes of heart failure are:
- Ischemic heart disease (coronary blocks/angina/infarction)
- Hypertension
- Valve problems of the heart
- Cardiomyopathy (heart muscle weakness)
The complaints typically given by patients are excessive tiredness, breathlessness, reduced ability to do physical activities, swelling of feet, cough at nighttime and discomfort in lying down posture. The cough, swelling of feet etc are caused by accumulation of fluids in the lungs and extremities as a result of the poor pumping of the heart.
While an X-ray chest will often show an enlarged heart and an ECG will show electrical changes, the ejection fraction (EF, an important parameter measured during an echocardiogram) gives a clear indication to the doctor about the cardiac function. The EF in healthy adults is between 50-75%, which means that the normal heart pumps just over half the heart’s volume of blood with each beat. There are 2 types of heart failure based on whether the EF is preserved (50% or more) or reduced (less than 50%). Both types of heart failure can be managed with medicines, limiting fluid and salt intake, and a proper diet and exercise regimen.
How does exercise help heart failure?
This is a very important question and warrants a thorough explanation. When someone is newly diagnosed with heart failure, they will be prescribed specific drugs to help improve the cardiac function and to reduce the symptoms. The number and dosage of drugs will be adjusted in the ensuing days to weeks until the symptoms are under control and the vitals are stable. Simultaneously, there will be changes made to the dietary pattern and fluid intake to prevent the heart from getting overloaded. This is the right time to initiate cardiac rehabilitation and supervised exercise as it benefits the heart in the following ways:
- Strengthens heart and cardiovascular system
- Reduces your blood pressure
- Helps manage your weight better
- Improves your circulation and the way your body uses oxygen
- Gives you more energy, which lets you be more active without getting tired or short of breath
- Makes your muscles stronger and more toned
- Prevents the heart failure from worsening
- Graded exercise improves the conditioning of your heart and lungs and allows you to participate in social, physical and sexual activities like normal individuals
While aerobic exercises are a must, strengthening exercises and balance and flexibility exercises are ideal too. It is recommended that individuals with heart failure keep track of how they feel during the exercise session and even after the session. Any excess breathlessness, discomfort, sweating, palpitation, giddiness or disorientation has to be informed to the healthcare provider immediately. Proper warm-up and cool-down are mandatory before and after each exercise session to prevent complications.
The advantages of a cardiac rehab program are that in addition to an exercise expert, there is a dietician who helps plan the meals and fluid intake per day taking into account the various factors like cardiac, renal and metabolic function; and there is a counselor who takes care of the psychosocial aspects such as feeling depressed, unduly stressed or helpless.
So how often should the EF be measured in someone with stable heart failure? The echo test, ECG and blood investigations should be done yearly if there are no new complaints, and more frequently if the clinical condition demands it.